BACKGROUND
ACT, which stands for Anticipatory Care Tool, is the product of a research project at University for the Creative Arts funded by Innovate UK in their Zinc Catalyst Healthy Ageing strand. It began in 2023 and is led by two UCA academics, Dr Harry Whalley and Mark Brill.
Along with other experts, we began working to help people living with dementia in 2018 on a project called Memory Tracks. This made a unique connection between music and memory to create a tool that helped people living with dementia manage their daily tasks.
Whilst developing an app for Cognitive Stimulation Therapy, we became aware of the technique called anticipatory care. The principle is quite straight forward - by identifying small but significant changes in physical and mental welling, it is possible to reduce hospitalisations for people living with dementia.
Although anticipatory care is widely understood, and is included in the NHS Long Term Plan, the technique is often informal, especially where it involves family carers, non-clinical carers, or other professionals supporting with people living with dementia. Our aim with ACT, was to build a simple tool that was easy to use and accessible for anyone who came into regular contact with older adults, especially those living with dementia.

THE PROBLEM
Dementia is a significant problem in an ageing population. In the UK there are over 1 million people with the disease and it is expected to reach 1.6m by 2050 (Fernandez et al., 2022). Dementia cost the UK £38bn in 2023 and it is estimated to rise to £47bn by 2050, surpassing cancer and heart disease costs.
A big challenge is that 1 in 4 hospital beds occupied by dementia patients (Lakey, 2019) and of those, 20% can be prevented if changes in wellbeing are spotted early enough (UK Gov, 2015 updated 2019). Studies have found that anticipatory care can reduce unscheduled hospital admissions for older adults (Baker et al., 2012), which gives a saving £2912 per person on average (Leckcivilize et al., 2021). It’s not just about saving money though. Older adults tend to stay in hospital for longer, 20 days on average, which leads to issues of bed blocking and it also disrupts the continuity of care at home. For example, people receiving care at home may not have the same carers when they come out of hospital and if no one is available they will be admitted to a care home. All of these issues contribute to reducing the wellbeing and quality of life for a person living with dementia.
WHAT IS ACT?
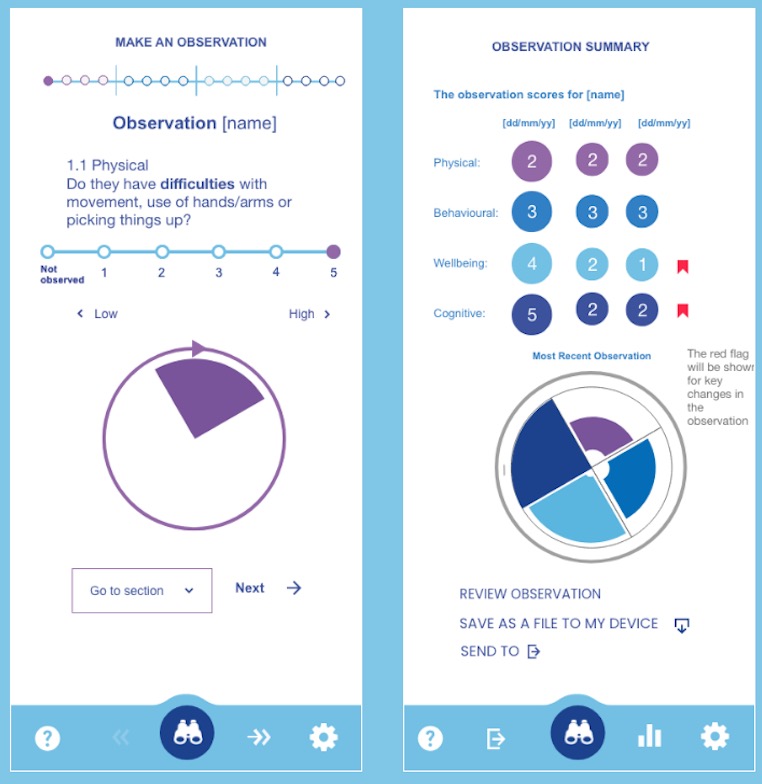
The Anticipatory Care Tool is for all! It is an app that can be used on any connected device (mobile phone, tablet or PC) for anyone who is caring for, or in regular contact with a person living with dementia. It is intended as an observational tool to help identify changes in wellbeing but rather than providing a diagnosis, it highlights key changes in health and wellbeing that enable referrals health services. It is non-clinical tool that does not require any specialist knowledge, although health professionals may also find it helpful. As a digital tool it can be used both online, such as during a video call, or in person.
HOW HAS IT DEVLOPED?
At the core of ACT are 16 observational questions split into four sections that cover physical health, wellbeing, behavioural and cognitive questions. The 16 questions are the result of research that considered 8 different professional tools, as follows:
-
Six-item Cognitive Impairment Test (6CIT)
-
Addenbrooke’s Cognitive Examination-III (ACE-III)
-
Comprehensive Geriatric Assessment (CGA)
-
NHS Dementia Diagnosis Toolkit
-
GST-4 Gait Speed Test
-
PRISMA-7
-
Clinical Frailty Scale (CFS)
-
Scottish Patients at Risk of Readmission and Admission (SPARRA)
Using this range of tools, the Research Team mapped the similarities and differences to identify the most important elements of the observation tool. Additionally, and as part of a co-design approach, workshops and interviews were carried out with Memory Matters in Plymouth and Lifecare in Edinburgh to further understand how effective observations could be made.
HOW ACT WORKS
To make an observation, the user firsts select the name or reference of the person they want to observe. If it is someone they haven’t observed before, they can add their name or reference into the system. They can also add a short note for that person. Once the person has been added to the system, they can make an observation by working through the 4 sections and 16 questions. Each question uses a simple scale from 1-5, where 1 is of the lowest concern and 5 is the highest. If they cannot make an observation for a particular question, they can simply skip to the next one and it will not be counted in the assessment. They can move back or forward through each section or jump from one to another.
THE ACT ALGORITHM
Particular observations will have different impacts on health of wellbeing of a person. In order to give appropriate weight to these observations, we developed the ACT Algorithm which reflects the differences in values for each question or section. There is also a red flag system to quickly identify deteriorations based on a moving average. The algorithm can be adjusted by ACT in order to reflect further feedback and research.
Using the ACT Algorithm as our base, we can add AI in the form of Machine Learning to the system through a time series prediction. The aim is to support the human observer to help provide a more anticipatory approach to the system.
OUR NEXT STEPS
ACT has been developed with the potential to plug it into other software via an API such as care management systems (CMS). The integration will be available as a licence model. ACT is also flexible itself and other enhancements can be easily plugged in. We will be bringing more AI into the tool that includes the use of computer vision and semantic analysis to further improve the observations.
CONTACT
For support or help enquiries relating to using ACT, please contact support@anticipatory.care
For enquires relating to our research, development or investment please contact hello@anticipatory.care